
A concussion protocol is an organization’s set of policies, tools, and assessments for caring for a concussion. It outlines how the concussion care team prepares for and responds to this injury. You may think a “concussion protocol” implies a strict, written policy that instructs healthcare providers to treat every patient and every concussion the same. However, trained healthcare providers know that a concussion requires an individualized care approach. For the purposes of this article, “protocol” and “policy” mean the same thing.
A concussion protocol (policy) is used to ensure everyone involved knows what to do when a concussion happens.

An organization needs a concussion protocol when they have children or adults who may be at risk for a concussion. Keep in mind: concussions don’t just happen in sports. They can happen at work, in auto accidents, or from falls. They happen to young children, adolescents, and adults. Learn more about concussions beyond athletics.
Most states in the United States have laws requiring schools to have protocols for their athletes. Ontario, Canada has also passed legislation requiring removal from sport and return to activity protocols for youth athletes. These laws are a step in the right direction to ensuring proper care after a concussion. However, there are still many countries and communities that lack written concussion protocols.
The person responsible for creating a concussion protocol depends entirely on the individual setting. In general, a healthcare provider familiar with concussions should be the one to create the protocol.

The best concussion protocols involve a variety of teammates and care stakeholders. At a minimum, a concussion protocol should involve at least these individuals:
Once you have your concussion care team assembled, make sure they have the training they need. Use our library of training courses to ensure everyone is on the same page when it comes to concussion care.
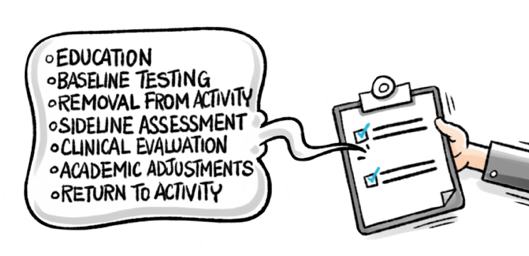
While concussion protocols differ by setting, most healthcare providers agree on the key concussion protocol steps that should be included. Concussion protocol requirements can also differ depending on country, state, or local laws.
At a minimum, concussion protocol steps should include:
With all these key elements, you’ll have a great start to a concussion management protocol.

Sideline evaluations are a critical early measure in checking for a concussion and determining next steps in the concussion care process. After a bump, blow, or jolt to the head, a healthcare provider trained to recognize concussions should follow a well-defined sideline process.
Athletic trainers are frequently the first responders in the case of an athletic head injury. Learn about their important role.
Because a concussion often happens without an athlete losing consciousness, a healthcare provider must use screening for head injury in other ways. Without a full sideline assessment, student athletes may return to play prematurely and be at risk for negative consequences. The brain can swell and cause lasting damage or increased long-term symptoms.
A sideline evaluation should include a symptom check and memory screening, cognitive functioning, and concentration. Its purpose is to determine if a trip to an emergency department is necessary. If not, they’ll determine if removal from participation with continued monitoring is warranted.
Brief tests like ImPACT Quick Test can help a healthcare provider quickly check cognitive function. Sideline professionals should also be on the lookout for worsening symptoms.

A concussion screening is a brief evaluation conducted by a trained healthcare provider. Its purpose is to determine the presence of a concussion after a blow to the head.
A trained healthcare provider will document whether or not there was a hit to the head and the location of impact. They will check for visible injury to the head or body. They’ll record if there was loss of consciousness, amnesia before or after the event, and any early concussion signs.
They will ask the patient about any symptoms they feel. They’ll likely conduct a brief cognitive screening to help make the removal from activity decision. They will determine if the patient requires an emergency department visit. The healthcare provider will continue monitoring for any new symptoms that might appear after the injury.

A baseline test measures your brain function in a healthy state. If you have an injury, healthcare providers can use a post-injury test to help determine if you have a concussion. It measures reaction time, memory capacity, speed of mental processing, and executive functioning of the brain. Baseline testing is recommended to be completed annually to ensure an up-to-date record of a patient’s normal functioning.
A trained healthcare provider can compare a post-injury test to a patient’s baseline. This way, they’ll have an objective idea of the extent of the injury. While concussions aren’t preventable, baseline testing is a great way to ensure someone is prepared if a concussion ever happens.
If you don't have time or resources to group baseline test all your test takers, you have two other time-saving options:

It measures the same areas as baseline testing. Healthcare providers use post-injury testing to understand a patient’s cognitive functioning after a jolt to the head. A post-injury clinical report is compared to a patient's baseline to show deficits in cognitive functioning and reaction time.
Post-injury testing can still be used if a test taker doesn’t have a baseline. This is thanks to normative data, which provides average scores within an age range. Post-injury testing is done by trained healthcare providers who use the test and other data to help evaluate a concussion. They’ll use it to develop an appropriate treatment plan to provide the most efficient recovery pattern.
Sandbagging is when a test taker deliberately underperforms on a baseline concussion test. Many athletes are aware that their ability to return to activity is determined by their baseline results. They may perform poorly to lower the threshold of comparison when their healthcare provider is deciding whether or not to clear them. It is not easy to sandbag during baseline testing because of built in validity indicators that flag suspicious results.
Read more about sports concussions and sandbagging as well as the preventative measures you can take.